CLINICAL PREDICTORS OF LONG-TERM MORTALITY AFTER FIRST ABLATION OF VENTRICULAR TACHYCARDIA IN PATIENTS WITH STRUCTURAL HEART DISEASE
Background
Catheter ablation is a well-established treatment modality for a wide spectrum of ventricular tachycardias (VTs). However, in the presence of structural heart disease (SHD), the prognosis and long-term mortality remains poor.
Objective
The aim of this study was to investigate the predictors of all-cause mortality after SHD-VT ablation in a high-volume expert center.
Methods
We evaluated 1143 patients (age: 63 ± 13 years, males: 87%, ICM: 67%, ES: 25%, NYHA Class: 2.1 ± 1.0, LVEF: 34 ± 13%, DM: 32%, COPD: 12%) who underwent first ablation for SHD-related VT between August 2006 and December 2020. Univariate and multivariate Cox-regression analyses were used to assess the predictors of all-cause mortality.
Results
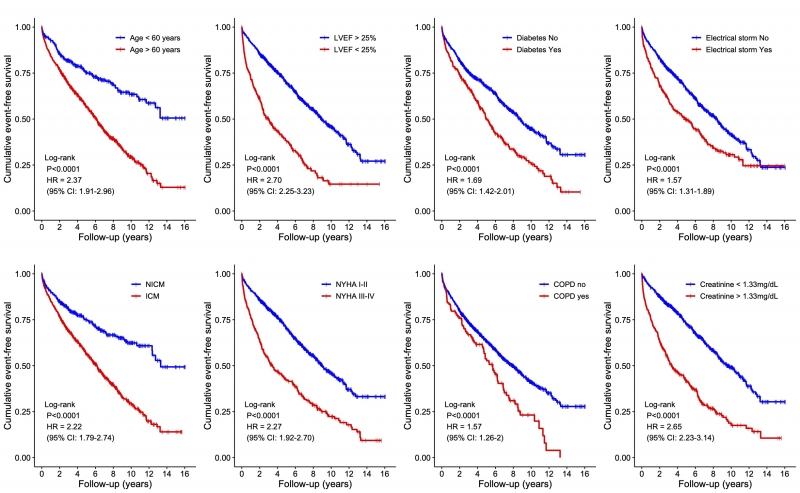
At mean follow-up of 4.1 years (IQR: 2.0 – 7.2yrs) an all-cause mortality was 48%. A total of 320 patients (28%) underwent repeated VT ablation. The averaged PAINESD score of our cohort was 11.4 ± 6.6 (median: 12, IQR: 6–17). Univariate Cox-regression analysis revealed eight parameters associated with poor mortality (Figure). After multivariate adjustment, only age >60 years (HR: 1.82, 95% CI: 1.4–2.2, p < 0.0001), ischemic cardiomyopathy (HR: 1.48, 95% CI: 1.1–1.8, p < 0.001), NYHA class ≥ III (HR: 1.6, 95% CI: 1.3–1.9, p < 0.0001), a serum creatinine level >1.3 mg/dL (HR: 1.7, 95% CI: 1.4–2.0, p <0.00001), LVEF ≤25% (HR: 2.2, 95% CI: 1.8–2.6, p < 0.00001) and diabetes mellitus (HR: 1.4, 95% CI: 1.1–1.6, p < 0.001) were strong and independent predictors of mortality.
Conclusion
In a large cohort of patients after SHD-VT ablation, an advanced age, poor ejection fraction, ischemic cardiomyopathy, high NYHA class and diabetes mellitus but not electrical storm or COPD were independent and strong predictors of long-term all-cause mortality.