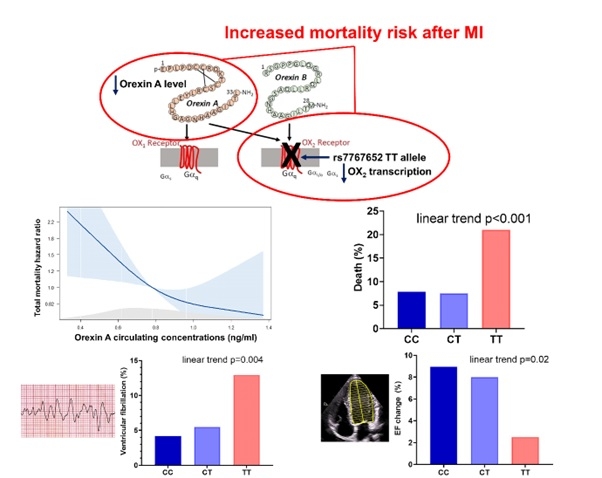
ATTENUATION OF HYPOCRETIN/OREXIN SIGNALING IS ASSOCIATED WITH INCREASED MORTALITY RISK AFTER MYOCARDIAL INFARCTION
Aims Hypocretin/orexin system has been shown to play a role in heart failure. Whether it also influences myocardial infarction (MI) outcomes is unknown. We evaluated the effect of rs7767652 minor allele T associated with decreased transcription of the hypocretin/orexin receptor-2 and circulating Orexin A concentrations on mortality risk after MI.
Methods Data from a single-center prospectively designed registry of consecutive patients hospitalized for MI at a large tertiary cardiology center were analyzed. Patients without previous history of MI or heart failure were included. A random population sample was used to compare allele frequencies in the general population.
Results Out of 1,009 patients (aged 64±12 years, 74.6% males) after MI, 6.1% were homozygotes (TT) and 39.4% heterozygotes (CT) for minor allele. Allele frequencies in MI group did not differ from 1,953 subjects from general population (χ² p=0.62). At index hospitalization, MI size was the same, but ventricular fibrillation and the need for CPR was more prevalent in TT allele variant. Among patients with EF≤40% at discharge, TT variant was associated with a lower increase in left ventricular EF during follow-up (p=0.03). During the 27 months of follow-up, TT variant was independently associated with increased mortality risk (HR 2.83, p=0.001). Furthermore, higher circulating Orexin A concentration was independently associated with a lower mortality risk (HR 0.41, p<0.05).
Conclusions Attenuation of hypocretin/orexin signaling is associated with increased mortality risk after MI. This effect may be partially explained by the increased arrhythmic risk and the effect on the left ventricular systolic function recovery.