PREDICTION OF SINUS RHYTHM MAINTENANCE USING CLINICAL PARAMETERS FOLLOWING ATRIAL FIBRILLATION ABLATION WITH PULSED-FIELD AND RADIOFREQUENCY ENERGY
Introduction
While pulsed-field ablation (PFA) and radiofrequency ablation (RFA) are effective techniques for atrial fibrillation (AF) treatment, predictors of long-term sinus rhythm (SR) maintenance remain unclear. We aimed to identify clinical predictors of 12-month SR maintenance in patients undergoing AF ablation with PFA or RFA.
Methods
In this prospective cohort of 386 patients (260 PFA, 126 RFA) treated between January 2022 and December 2023, logistic regression assessed the association between baseline parameters and 12-month SR maintenance. Follow-up included at least one 24-h Holter in the first 6 months, one at 12 months, and two outpatient visits. Predictors from univariate analysis were age, sex, weight, BMI, ischemic heart disease, hypertension, ejection fraction, left atrial size, AF type, diabetes, and ablation type. Models were built for the entire cohort and separately for PFA and RFA.
Results
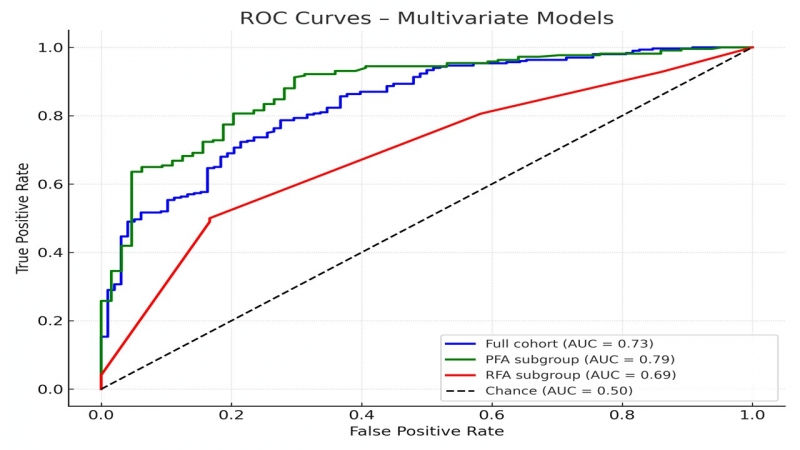
In the full cohort, higher age (OR 0.96; 95% CI 0.93–0.99; p = 0.007), weight (OR 0.97; 0.96–0.99; p = 0.003), ischemic heart disease (OR 0.51; p = 0.12) and persistent AF (OR 0.50; p = 0.03) predicted lower SR maintenance (AUC 0.73).
In PFA patients, higher age (OR 0.92; p < 0.001) and weight (OR 0.96; p < 0.001) were significant (AUC 0.79).
In RFA, persistent AF (OR 0.41; p = 0.04) and beta-blocker use (OR 2.98; p = 0.02) were significant (AUC 0.69).
Conclusion
Age, weight, AF type, and some structural parameters are key predictors of AF recurrence after ablation. Predictive accuracy was higher for PFA than RFA, supporting technology-specific risk stratification to guide patient selection and improve long-term outcomes.