CHRONIC OBSTRUCTIVE PULMONARY DISEASE IS A RISK FACTOR FOR VENTRICULAR ARRHYTHMIAS INDEPENDENT OF LEFT VENTRICULAR SYSTOLIC FUNCTION
Background and Aim:
Chronic obstructive pulmonary disease (COPD) is associated with increased cardiovascular morbidity and mortality, yet the exact pathophysiological links remain unclear. Whether the presence and severity of COPD is associated with ventricular tachycardia (VT) independent of the left ventricular ejection fraction (LVEF) remains unknown.
Methods:
We identified consecutive adult patients who underwent pulmonary function testing, 24-hour Holter monitoring, and trans-thoracic echocardiography between 2000 and 2009. Demographic data as well as relevant co-morbidities were gathered from the electronic medical record, severity of COPD was classified according to the GOLD classification, VT diagnosed as ≥3 consecutive ventricular beats at a rate >100/minute.
Results:
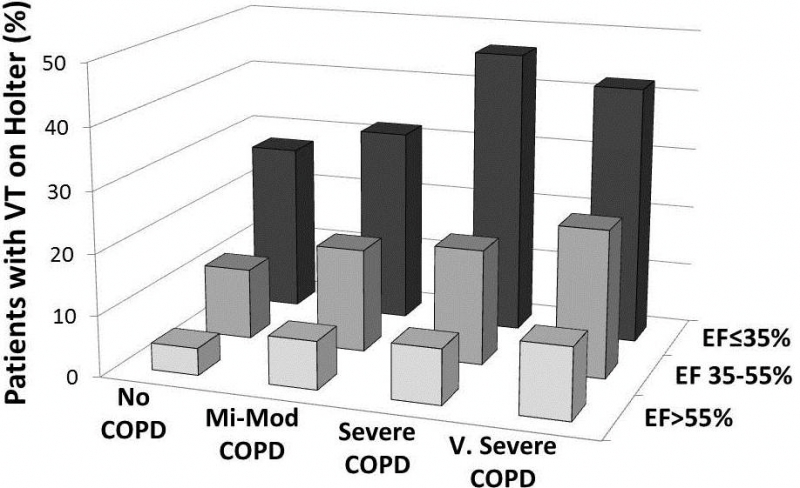
From 6350 patients who were included (age 66±15 years, 48% woman, 92% Caucasian, LVEF 59±12%) COPD was diagnosed in 2799 (44%). COPD was associated with a nearly two-fold increase in likelihood of VT occurring on the Holter monitor (6.9% vs 13.7%, p<0.001). The severity of COPD was also predictive of the risk of VT (12.2% vs. 16.7% vs. 20% for mild-moderate, severe, and very severe COPD, respectively; p<0.001). COPD and VT remained independently associated (p<0.001) after stratifying for LVEF (Figure), demographics, and co-morbidities (age, gender, tobacco use, obesity, hypertension, coronary artery disease, heart failure, diabetes, chronic kidney disease).
Conclusions:
COPD is associated with increased risk of VT, proportionate to severity and independent of the LVEF. This provides insight into the markedly increased cardiovascular mortality of COPD patients, and further studies should explore which anti-arrhythmic strategies would best apply to the COPD patients.