VIEW AN ABSTRACT
EARLY AND DELAYED ALTERATION OF LOCAL ATRIAL ELECTROGRAMS AROUND SINGLE RADIOFREQUENCY ABLATION LESION
Topic: field | |
| Type: Presentation - doctors , Number in the programme: 151 | |
| Havránek Š. 1, Alfrédová H. 1, Fingrová Z. 1, Bulková V. 2, Bouček T. 1, Součková L. 1, Wichterle D. 3 1 II. interní klinika, VFN Praha, Praha, 2 Centrum kardiovaskulární péče Brno, Interní kardiologická klinika FN Brno, Brno, 3 Klinika kardiologie, Institut klinické a experimentální medicíny, Praha | |
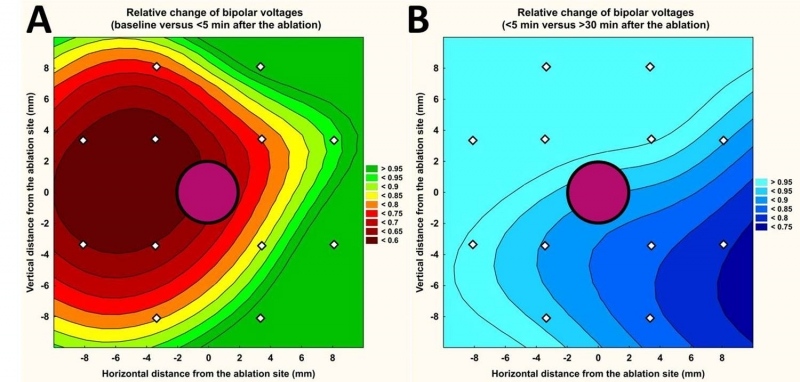
Purpose: The acute effect of radiofrequency ablation consists of local necrosis, collateral stunning and oedema. We investigated the spatiotemporal change of atrial electrograms in the area surrounding the site at which single standardised pulse of radiofrequency energy was delivered. Methods: The study enrolled 14 patients (61 ± 10 yrs, 9 males) with paroxysmal atrial fibrillation undergoing ablation procedure with irrigated-tip ablation catheter and 3D navigation. The high-density mapping / remapping (129 ± 63 points) with radius of ~10 mm, centred at the pre-specified posterior left pulmonary vein antrum ablation site was performed at baseline, immediately after single radiofrequency energy delivery (25 W, 30 s, 20 ml/min) and after 30-min period. Bipolar voltages of atrial electrograms (A-EGM-biV) were averaged within the central and 12 adjacent left atrium segments and their relative change was studied. Results: After the ablation, overall A-EGM-biV within the mapping zone (2.4 ± 0.65 mV at baseline) reduced to 1.87 ± 0.94 mV (immediately) and to 1.67 ± 0.75 mV (after 30-min period). In per-segment pair-wise comparison, we observed highly significant change in A-EGM-biV that extended up to the distance of 8.8 mm from the lesion core. The maximum early A-EGM-biV attenuation by 39 – 49% (P <0.001) was registered in segments adjacent to pulmonary vein ostia (Figure, Panel A). The subsequent (delayed) A-EGM-biV reduction by 17 – 24% (P <0.05) was observed in opposite direction from the lesion centre (Figure, Panel B). Conclusions: Significant alteration of atrial electrograms was detectable rather distant from the central lesion. Spatiotemporal development of ablation lesion was excentric / inhomogeneous. While acute A-EGM-biV reduction can be attributed to direct thermal injury, delayed effects are probably due to oedema progression. | |
 |
 česky
česky
